Spip FAQs
For practice managers
Everything your clinicians need to know to manage patients in your practice.
What is an 'Organisation' in Spip?
Organisation is one of the four different types of Cudos item.
- an establishment that has more than one Internal department, service or policy and/or Individual or role within it e.g. a GP surgery, hospital, community trust etc.
- offers services via Internal departments, services or policy.
- is based at one postal address.
- you will probably only have a few of these.
Do you have Spip video tutorials?
Yes. We have a growing list of Spip help videos and tutorials.
What are the Practice, Staff, Clinician and Editor roles in Spip?
The Practice is the lead role in Spip. This person will have authority from the practice to create a Spip and an NHS email address. They will usually be a practice manager or another senior member of the practice team.
The Practice is able to:
- add and edit items to Spip and Cudos.
- manages other users of Spip and Cudos.
The Practice can invite or deactivate Clinicians:
- The Clinician role can view Spip.
- Clinicians can be any clinician working in your practice who can benefit from access to Spip e.g. practice-based GPs, GP locums and nurses.
The Practice can invite or deactivate Staff:
- Staff can view Spip and Cudos. Cudos may contain items that are just for use by your practice staff e.g. building maintenance, IT system support, health and safety protocols. You would not want to display these in Spip but you can make them accessible to your practice staff by setting them up as Staff roles.
Practice can invite Editors.
- The Editor role can view Spip and Cudos but also add or edit items in Spip or Cudos.
- Editors will usually be established members of your practice team who are entrusted to share their knowledge of practice procedures and services with Clinicians, via Spip, and with Staff via Spip and Cudos e.g. GP partners, medical secretaries and nurse practitioners.
Switching roles
The Practice can switch people between different roles e.g. upgrade a Clinician to an Editor so they can crowdsource their knowledge of services
How do I use Spip messaging, comments and notes?
Simple, yet powerful
Spip comes with its own messaging, comments and notes system. It’s a great way for all members of a practice – including visiting locum GPs – to share local information about service quality.
If you have any unread messages, we’ll send you an email at 2pm to let you know, allowing you to go straight to your messaging area.
Comment on this page
All users can comment on any page within any Spip they have access too – advice to colleagues, useful tips etc.
That comment will only be visible on that particular practice’s Spip. A copy is sent via the Spip’s messaging system, and the Practice can edit the comment.
Leave a personal note
Useful for Clinicians to leave a personal note about that service for themselves. Only the person who made that note can see it.
Unlike ‘comments’, personal notes will be visible in all other Spips (on that specific page) – but again, visible only to the person who created that note.
Report service issue to Practice
Great for flagging up issues to a Practice about a service, enabling them to collect and escalate these issues further to prevent them happening again.
You must never include any patient-identifiable information in these reports.
Request page update
If you’ve looked something up in Spip but couldn’t find it, or something was out-of-date or wrong, this lets the practice know.
What is a Spip ‘Editor’?
The owner of a Spip – ‘Practice’ – can upgrade a Clinician to an Editor.
In addition to everything a Clinician can do, an Editor is also able to populate and edit Spip itself, keeping it up-to-date and relevant.
A Practice can invite as many Clinicians or Staff as it likes to help it ‘crowdsource’ information.
It’s easy to downgrade an Editor back to a Clinician.
Getting started with Spip (GP practice guide)
If you are creating a Spip you are probably taking on the Practice role.
The Practice is the lead role in Spip. This person will have authority from the practice to create a Spip and need an NHS email address to register their practice. They will usually be a practice manager or another senior member of the practice team.
However, an interested Clinician can make a start on creating a Spip (with the practice’s permission), by the practice manager changing their role within Spip to Editor.
Spip | What are the Practice, Staff, Clinician and Editor roles in Spip?
Spip | Who can see the information within Spip and Cudos?
Think of Spip (Standardised practice induction pack) as a standardised, easy to search display cabinet. You populate Spip by responding to queries set out in the standardised template.
Much of the information you add will be stored in Cudos (Centrally updatable directory of services)
To begin Spip’s QuickStart, in Spip navigate to The practice >> Getting here >> The practice.
What is a Spip ‘Individual or role’?
Individual or role is one of the four different types of Cudos item.
- is any single person.
- doesn’t need an actual name; can be just entered as their role.
- can be someone from an Organisation, an Internal department, service or policy or from a Single service or premises.
- can also be added without associating them with any of the above.
- e.g. like you, any GP or staff member in your practice.
What is a ‘single service or premises’ in Spip?
Single service or premises is one of the four different types of Cudos item.
- exists to provide only one type of service e.g. your local pharmacy, counselling service, or perhaps a physiotherapy clinic.
- may have Individual or role within the service, but no Internal department, service or policy and is not part of an Organisation.
- is based at one postal address.
What is a Spip ‘Internal department, service or policy’?
Internal department, service or policy is one of the four different types of Cudos item.
- is always part of an Organisation e.g. diabetic clinic within a GP surgery, ENT unit within a hospital or community podiatry service as part of a community trust.
- shares a postal address with their parent Organisation.
- can also be a pathway of policy within an Organisation e.g. complaints procedure or a care pathway.
LocumDeck | Compatibility and security
The entire NASGP website, including Practeus and its associated components LocumDeck, is hosted on a dedicated server, using ISO 27001 and ISO 9001. All data during transmission is encrypted and authenticated using AES 128 GCM and uses ECDHE RSA as the key exchange mechanism.
You do not need to download any software.
If you’re able to, we strongly recommend you upgrade to a modern browser like Google Chrome, Edge, Firefox or Safari to run alongside IE 10 if it’s still needed for NHS legacy websites.
Payment processing
- We do not accept, store, transmit or process cardholder data or any payments. We subcontract all these sensitive payment handling activities to third parties, GoCardless for direct debit payments and Nochex for credit card payments, all of who comply with PCI DSS Standards.
Firewall, security and encryption - Our site uses SHA-256 with RSA Encryption
Cloud server
- LocumDeck is on a dedicated server, which is ISO 27001 security compliant.
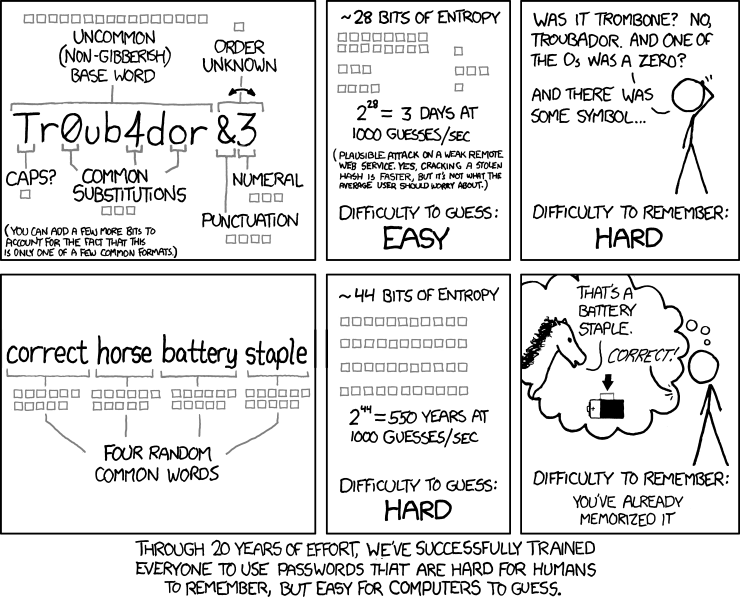
Using passwords
The latest advice is to ditch using complex letter/character combinations, and use passphrases instead.
New NIST guidelines recommend using long passphrases instead of seemingly complex passwords. A passphrase is a “memorised secret” consisting of a sequence of words or other text used to authenticate their identity. It’s longer than a password for added security but much easier to learn.
Create unique passphrases you can remember, using whatever characters they want. e.g
- Honeymoon beach flower ketchup
- Correct horse battery staple
Is Spip mobile-friendly?
Yes. A Clinician can use Spip from a smartphone using wifi or data (3G or 4G).
Can I get my local ‘Network’ to update my Spip?
The best way to get your CCG, federation, GP hub or hospital helping you is to use the ‘Network‘ invitation (coming summer 2016) function within your Spip Dashboard. This is where a Practice can invite a parent organisation e.g. CCG, GP federation etc to create its own central Network-Cudos, whose information can also be viewed, copied or synchronised by practices, and allow practices to integrate Network-Cudos information across its own Spip together with practice-specific information from the practice’s own internal Cudos.
Will any third parties be able to see our Spip data?
Never. The only other people authorised to view your practice’s information are the NASGP’s clinical directors, who will from time-to-time monitor how practices are using their Spips so that NASGP can continually improve Spip.
NASGP is registered with the Data Protection Act.
Who owns Spip information?
All information and data added by a practice to a Spip and its corresponding Cudos belongs to that practice. See our Terms and Conditions for more information.
Spip | Who can see the information within Spip and Cudos?
This all depends on what role the Practice has assigned you.
| Role | Spip | Cudos | Group’s Cudos | Explanation |
|---|---|---|---|---|
| Practice | Own & Edit | Own & Edit | View | A single authorised person within the practice who controls and manages Spip and Cudos. Can add and delete contacts in Cudos and content in Spip; can invite anyone to be a Clinician and change the status of Clinician to Editor or Staff. Can also invite and activate Group. |
| Editor | Edit | Edit | View | Same as Clinician; can also add and delete contacts in Cudos as well as in Spip. |
| Staff | View | View | View | Same as Clinician; can also view Cudos. |
| Clinician | View | Hidden | Hidden | Can view all content in Spip that has been authorised for viewing by Practice or Editor. Can not directly view Cudos. |
| network | Dummy | Hidden | Edit | Can only be invited by Practice; can add and delete contacts in a separate Network Cudos. Can not view any contents in Spip. By inviting a Network (e.g. a single contact at a CCG or a GP federation) to add and delete contacts in a separate network Cudos; Practice or Editor can choose to also use contacts that have been added by Network. |
What is Cudos?
Cudos stands for ‘Centralised Updatable Directory of Services‘ and is like a smart address book designed specifically for general practice. Unlike a regular address book, it allows for one item (e.g. a person, service or policy) to be linked to another item (e.g. a practice or hospital)in a specific way.
- By creating a relationship between items, it greatly reduces the need for duplication, enabling the information to be always as up-to-date as it can be.
- Cudos also allows you to attach enriched information and resources to each item.
- You can link, upload or otherwise direct users to referral forms, policies and care pathways.
- Any item that you’ve created in Cudos and then selected for display in Spip can be edited in either, and changing one always reflects the change in the other.
- By following the Spip-Tips throughout Spip, the Practice role can create and present any of this stored information at any point throughout Spip.
- All this information is then presented to the Clinician role at the point of need in the appropriate places throughout Spip.
- Although Spip is by far the best place to quickly look up information, the Practice can also enable users associated with your practice to be an Editor or Staff who are able to directly access Cudos.
Cudos has four different types of item:
Organisation
- Like your practice or a hospital. You’ll only add a few of these.
Internal department, service or policy
- Anything from your surgery’s asthma clinic to a hospital’s x-ray department. It can also include any policies used by that organisation, such as a complaint’s policy.
- You can also upload documents or add links.
Single service or premises
- Like a local pharmacy, physiotherapist or dentist. You’ll only add a few of these.
Individual or role
- Like you, any GP in your practice, and hospital doctor – whether by their name or by their role.
What is Spip?
Spip is NASGP’s Standardised Practice Induction Portal. It is a secure online platform that enables a practice team to centrally store and safely display essential information to enable any clinician working in any of its premises to manage patients quickly, effectively and efficiently.
It is not linked to your clinical IT system (EMIS, SystmOne etc) and does not contain any patient-identifiable information, so can be shared with any locums visiting your practice and can be accessed from home and on home visits. Within Spip you will find a centrally updatable directory of services – Cudos.
How do I set up branch surgeries in Spip?
Branch surgeries can easily be accommodated within Spip.
Small single-use branch
If a branch is used for the sole purpose of consulting, and all other activity such as blood tests happens elsewhere, then consider adding this branch as a Single service or premises.
Larger multi-use branch
These branches would include other services like phlebotomy, maybe have a treatment room or possibly many other services, in which case we recommend setting up this branch surgery as an Organisation. But otherwise, this branch surgery operates pretty much as it’s larger ‘parent’ practice.
Large multi-use branch, operating semi-independently
You’re gonna need a bigger boat. As you already have a Spip with us, please get in touch and we’ll be able to arrange another license for you.
How much does Spip cost?
Starting August 2016, Practice Manager membership of the NASGP is now free. Spip comes free with that membership.
Spip has the additional capability to link with any local networks (CCGs, federations, practice hubs etc), for which that network will pay a small monthly charge of no more than £24 for each practice it links to.
It’s also always free to Editors, Clinicians and Staff.
A Practice can:
- Add as many Editors, Clinicians or Staff it needs; although all users have to sign in with an email and a password, they will never have to pay to join the NASGP.
- Cancel their membership at any time.
- Ask us to remove all their data at any time, otherwise we will automatically remove all Spip data after one year. A Practice, and therefore all its Clinicians, Staff etc can re-access its Spip at anytime simply by rejoining.
How does Spip help clinicians work better?
When it comes to managing a patient in a GP surgery, we need access to one of atleast 200 items of information that are specific to that practice. If we can’t recall this from memory, or it’s not immediately accessible, retrieving this information can waste precious minutes or even hours of our time, a colleagues time and , most importantly, our patients time and even put a patient’s health at risk.
It’s those 200 bits of local, practice-based, non-clinical information that Spip enables practices to provide for all clinicians caring for their patients:
- How do I organise an urgent ECG in the middle of a busy surgery?
- What do I tell a patient about how they will be informed of abnormal blood tests?
- Which helicobacter pylori test is used at this practice?
- I’ve seen a nine year old boy with suspected testicular torsion who needs emergency referral. Which team do I refer him to?
- The local DVT pathway says ‘Do a D-dimer test’. How is this done at this practice?
- Where are echocardiograms carried out? How do I request one? What do I tell the patient about the appointment-making process?
- I’ve requested a chest x-ray on a 68 year old man with a cough. How do I alert his usual GP that he may have a significant diagnosis?
- What’s the extension number for main reception?
- Who’s the practice’s child safeguarding lead?
- I need a foreign language interpreter.
- How do I organise an urgent coil fitting as emergency contraception?
- What’s the door access code to the toilet?
Spip contains over 200 similar, simple-yet-essential everyday scenarios.
How long does it take to set up a Spip?
Step 1 (OPTIONAL*) | Network-Cudos – 4 hours initial setup, 20 minutes/week thereafter
- Performed by a Network (CCG, federation etc) employee (manager, administrator or clinical lead) who has oversight of where links and documents are published or stored.
- Accessible to unlimited number of the Network’s practices.
- Arriving Summer 2016.
- * If Network-Cudos not available, practice can add this information to their own Cudos – 2 to 4 hours initial setup, 10 minutes/week
Step 2 | Practice Cudos – 2 to 4 hours initial setup, 10 minutes/week thereafter
- ‘Simply’ transferring information from the practice’s address book to their practice’s Cudos.
- Performed by designated practice employee (user assigned as ‘Editor‘ by the practice manager).
- Unlimited number of practice staff who need to access information in Cudos, such as contacts and practice policies, can be assigned as ‘Staff’ by the practice manager.
Step 3 | Practice Spip – 2 hours initial setup, 10 minutes/week thereafter
- Performed by practice manager and/or other experienced manager.
- Selects which information to display from the Network-Cudos (if available) and practice’s own Cudos, and adding other relevant information specific to their practice.
Step 4 | Practice Spip – 1 to 2 hours review, 10 minutes/week collectively thereafter
- Performed by one or more practice GPs (users assigned as ‘Editors‘ by practice manager).
- Unlimited number of users who need to access any of this information for the purposes of patient care are assigned by practice manager as ‘Clinician‘.
How can Spip help me recruit GPs?
- A well organised and up-to-date Spip says a lot about how your practice supports all clinicians and staff to do their job safely, efficiently and effectively.
- They’ll have more time, and less stress. A survey we carried out in September 2015 about a typical morning surgery revealed that, on average, locum GPs spend 20 minutes, and GP partners 10 minutes, trying to find precisely the sort of information found in Spip.
To help practices recruit, we’ve produced a Spip logo that we encourage you to include with any correspondence with locums, add to your job adverts, and include on your website etc, to give assurances about the importance of giving clear information to your clinicians.
If we’ve already got DXS/Map of Medicine, why do we need Spip?
Think of Spip as the information air traffic control of your GP practice, while services like DXS and Map of Medicine are the different airlines. Information used in GP practices comes from many different internal and external sources, and DXS/Map of Medicine are only one of these, and are generally outside the control of the practice.
Spip is practice-specific, focused on enabling a Clinician at the point of use to run a safe, effective and efficient consultation, or a Staff member referring to up-to-date information about practice processes. This encompasses far more than is contained in a local guideline.
For example, a local guideline may simply state “Arrange urgent ultrasound scan”. Enacting this seemingly simple instruction will actually involve the Clinician having access to lots of bits of information about how your practice works:
- How do I organise an urgent ultrasound in this practice?
- Do I just send a form or do I also have to phone radiology?
- Where are the referral forms?
- How does this practice handle urgent referrals?
- What’s this practice’s policy on informing the patient of the results?
Spip:
- Is completely controlled by you and is centred around your practice rather than the CCG.
- Does not require an NHS smartcard, and is not integrated into the clinical system. So it can be accessed by any clinician from a smartphone or from home, during visits, and before visiting a practice for locum work for the first time – or any time!
- Uses a standardised format – all practice Spips have exactly the same structure – which is quick and easy to navigate, so you can direct Clinicians to key information about how your practice works and how you link up to local guidelines.
Can’t doctors just ask the receptionist?
They – being a GP, nurse, locum or new team member – could just ask the receptionist, but:
- The receptionist may not know the answer. Often this is the case, and a time-consuming game of “pass the parcel” ensues, taking up time of multiple staff. This is no bad reflection on anyone in the practice team; it’s just there’s so much to know and it’s always changing, so it is not reasonable to expect the duty admin team to be ‘know-it-alls’.
- It wastes time – not just the person seeking information (often a GP in the middle of a busy surgery), but the receptionists too.
- It undermines the GP-patient relationship: “If the GP doesn’t even know how to refer me to physiotherapy, how do I know she’s even made the correct diagnosis? I know, I’ll rebook to see another GP.”.
How do I create a Spip for a practice?
The person who initially sets up a Spip takes on the lead role, known as ‘Practice’, is responsible for administrative tasks such as managing other Spip users e.g. controlling who can view and edit Spip.
Therefore, usually the practice manager is best placed to initially set up a Spip by registering for Practice Manager membership of the NASGP.
Spip is included free as part of Practice Manager membership.
- You will need an NHS email address ending in
- nhs.net
- nhs.uk
- hscni.net
Once your Spip has been created, you can change your email address to a non-NHS email.
If you are a locum GP who wants to be involved in creating Spips for practices you work in, you can become a ‘Spip Clinician’ by registering with the NASGP as an Associate (free) or Full member. Once signed in, you will be able to ‘Invite new GP practice’ to create a Spip.
If you are a GP wishing to create a Spip for your own practice, unless you want to take on the administrative tasks of managing Spip users, the best route is to ask your practice manager to register for Practice Manager membership and set you up as a ‘Spip Editor’.
Why does my practice need a Spip?
NASGP’s Standardised Practice Information Portal (Spip) allows any practice to present all 200+ items of shared information immediately in front of all its clinicians at the point of patient contact.
Although every GP knows tens of thousands of ‘bits’ of clinical information that he or she can formulate into a diagnosis and management plan within minutes of seeing a patient, when it comes to managing that patient’s condition, they need to have access 200+ ‘bits’ of very localised non-clinical information about practice processes affecting safe patient management (e.g. managing test results, referrals, handover arrangements, prescribing procedures etc) and how the practice interacts with local resources.
Even for an established senior partner, practice processes, regulatory requirements and other local non-clinical information can change at a frightening pace, so having instant access to this information isn’t just a luxury but a central requisite of modern patient management.
It’s far safer, and more efficient, to spend two minutes updating information centrally in Spip than having a GP interrupt their surgery for 10 minutes to ask a staff member or another GP.
Now take into consideration the position of a locum GP, who can typically work in around 30 different GP practices every year, where in each of these practices, practically all these 200 ‘bits’ of non-clinical information can be alien to them. By enabling all clinicians caring for your patients to have instant access to your Spip, you’ll be empowering them to be better at what they do, and more efficient. No more time wasted having to interrupt the consultation to ask for simple but essential non-clinical information.
Locums may be most at risk of falling into pitfalls created by gaps in information about practice procedures but practice-based GPs and staff may also be prone to errors and misunderstandings. For instance, evidence from Medical Protection suggests that 57% of 107 practices undergoing a Clinical risk self assessment (CRSA) were found to have risky referral systems, often related to lack of understanding of referral protocols by practice staff and clinicians.
- Improve the quality of admissions and referrals by all clinicians who work in your practice, whether full-time, part-time or an ad-hoc locum basis, by making sure all this information is at their fingertips. Especially useful if you’re taking on a new partner, salaried GP or GP registrar.
- Increase efficiency by enabling any clinician or staff-member to access any piece of important information about patient management within 3 clicks of a mouse, whether they’re in surgery with a patient, at home or on a visit.
- Improve patient safety by publishing simple but important practice-specific procedures and safety-netting information for all clinicians and staff to relay to patients.
- Better value for money from ad-hoc staff and clinicians such as locum GPs and nurses; they can review your Spip before arrival, access it on the day, and they’ll be able to spend more of their time on direct patient care rather than having to bother busy members of staff.
- Satisfy the CQC that you are publishing essential information to all clinicians and staff who care for patients in your practice.
- Reduce errors by having this information in one central place that can be updated instantaneously.
What is Network-Cudos?
Network-Cudos (Centralised Updatable Directory of Services) allows any CCG, GP federation, practice hub or a provider to centrally populate its own relational database of records that then seamlessly integrate with any related practice’s Spip (Standardised Practice Information Portal).
To set up a Network-Cudos, you’ll need to sign up for it here. You’ll also then need to invite local practices to share it with, and they will have to accept your invitation.
By having a Network-Cudos, a CCG, GP federation etc can maintain a complete live database of all local organisations, departments, individuals, roles, services, guidelines, pathways and policies. Each of the Network’s practices can then choose any of the Network’s records to be displayed within its own practice’s Spip, and even customise some of the Network’s information for practice-specific use.
All of this extra functionality is in addition to a practice’s own Cudos and usual Spip.
Can Spip help with CQC compliance?
Yes. Spip is ‘CQC-ready’, with a dedicated section to easily categorise, store and display all your necessary policies.
Spip is a great way to demonstrate to the CQC that the right information is available at the right time to all members of your practice team to allow effective implementation of all your practice procedures. So Spip will not only provide you with a ‘go to’ place for your team to refer to and update information, in creating it, you will also making your CQC compliance less onerous.
See what the CQC has to say about Practice packs.
- Spip allows you to upload, link and add freetext notes for handy summaries and ‘soft intelligence’ about key practice operational procedures. It is a live, interactive, centrally updatable system designed to be easily searched and navigated.
- Once you’re up and running with Spip you will be able to show the CQC that your Staff and Clinicians need never be more than 3 clicks away from information they need.
- GPs can already access key practice policy information that directly affect them as Clinicians e.g. chaperone policy, complaints procedure, clinical handovers, appointment system and access arrangements, practice prescribing procedures, contamination incidents etc.
Managing risk and quality
Monitoring quality of services
- On every Spip page displayed to your team there is a feedback comment system with a prompt to report any problems with a service at the point of use. This intelligence can be collated by the practice for discussion at internal meetings and/or to be raised with the local commissioners and providers.
Patient communication and reducing risk
- Throughout Spip you are prompted to add detailed information about Safety netting, missing results procedures, delayed referrals etc.
- The aim is for everyone in the team to have this information available quickly so that after every patient contact, it is clear to the patient and the practice what is expected next.
Co-operation with other providers of services
Spip is designed to provide up-to-date information which the Clinician can access at the point of need. You have the option of adding enriched information about each service which would equip the Clinician with:
- Awareness of the existence of a service.
- Understanding exactly what the service does; the boundaries of roles and responsibilities between the service and the practice, fostering good team working.
- How to access the service and up-to-date resources to do this e.g. referral forms.
- What to tell the patient about what to expect next.
- Interactive feedback; ability to leave comments or tips for future Clinicians; ability to report a problem with the service; ability to inform you if service details need updating.
Who adds information to Spip?
The person who first signed up for the Spip – usually the practice manager, ‘Practice‘ – has full control over the information that appears in their Spip, as well as being able to input information themselves.
Practice, via their Dashboard, will also invite Clinicians to view their practice’s Spip, and can also reassign any Clinician to become an Editor.
Editors will usually be members of your practice team who are familiar with your practice procedures and local services e.g. GPs, medical secretaries, practice nurses. An experienced, trusted locum could also be a suitable editor. Editors can keep Spip up-to-date in the same way as Practice.
Even Clinicians can contribute to your Spip’s completeness by leaving comments on any Spip page.
How was Spip developed?
15 years ago, locum GP and NASGP chairman, Dr Richard Fieldhouse was named ‘Sessional GP of the Year’ by the Doctor newspaper. The award recognised his development of the inspired GP ‘Practice Pack’, in essence, a one-stop paper portfolio for busy GPs which could be updated with a practice’s key information, such as local referral pathways and vital admin information.
Fast forward to 2015 and the need for such readily accessible, highly localised and practice-specific information, is even more compelling as health care tends to be delivered by an ever-increasing and ever-changing array of services and teams. In the intervening years technology has transformed how such information may be stored, accessed and updated.
So Spip – a secure online platform inspired by the earlier paper version – has taken over two years for Sara Chambers and Richard Fieldhouse to develop. Both are sessional GPs with over 35 years collective experience of having worked in over 150 different GP surgeries throughout their GP careers.
MPS have supported the development of Spip and CQC have helped with advice.
What if I don’t have time to add information to Spip?
Research conducted by the NASGP found that, on average, GP partners spend 20 minutes a day, and locums 40 minutes a day, having to ask someone else for essential information about practice processes or how the practice interacts with other service providers. And then factor in the time of the person they’re asking who has been interrupted from their duties. And then the risks of delays, increased work and costs, and lapses in patient care if accurate, up to date information is not available.
And that’s just a GP survey. What would a similar survey of practice nurses and the administrative team reveal?
So a couple of minutes adding a practice policy, a useful contact or a care pathway could repeatedly save a clinician, a patient and other members of your practice team many multiples of the time it takes to add it.
Spip can help with CQC compliance so completing Spip could be seen as part of your CQC preparation – but with the added benefit that you’ll also be creating a live, easy access, interactive, centrally updateable information portal for all your team to refer to in their daily work.
It is not the intention that one individual will complete Spip all at once.
Some frequently-used or safety-critical items you may wish to add immediately. It’s likely that this core of around 20% of the items in Spip will be used 80% of the time, so for a relatively small investment of time – 2-4 hours – you could have a very useful Spip that will already be improving safety, saving precious time and reducing frustration for your over-stretched practice team.
Less commonly used items can be added “on the go” over time by your team of Editors. Some items you may decide never to complete if you feel they are not relevant to your setting.
- Others can help you crowdsource information.
- See our suggestions on how to prioritise adding information to Spip.
- This will allow a GP network, such as a CCG, to independently populate a Network-Cudos and make it available to local practices.
- After accessing a Network-Cudos item e.g. a care pathway, practices can add their own specific information about how that information is implemented in their practice.
Toolkit | Checklist for home visits
Home visits are some of the most complicated activities that GPs do. Away from electronic records, usually after a busy surgery, through traffic, to sick or frail patients, often with multiple problems and anxious carers.
Our template helps you make the whole process go much more smoothly.
Checklist for home visits
Download – Word Save as – Google Doc
See also
Toolkit | Restock consulting room equipment
The best person to let you know when a room needs reequipping is the last person that used it. Print some of these out and pin to each room’s notice board.
Restock consulting room equipment
Toolkit | Locum pre-arrival checklist
To get the most out of your freelance GPs and minimise stress to your practice staff and disruption for patients, it is helpful to have the following in place in time for your GPs to smoothly start their session.
Locum pre-arrival checklist
Download – Word Save as – Google Doc
See also – More tools for practices to support locums
Toolkit | Dictate referral template
These allow clinicians to make a physical record of every consultation that needs referral, reducing the likelihood of a referral going missing.
Dictate referral template
For clinicians
Everything your clinicians need to know to manage patients in your practice.
How was Spip developed?
15 years ago, locum GP and NASGP chairman, Dr Richard Fieldhouse was named ‘Sessional GP of the Year’ by the Doctor newspaper. The award recognised his development of the inspired GP ‘Practice Pack’, in essence, a one-stop paper portfolio for busy GPs which could be updated with a practice’s key information, such as local referral pathways and vital admin information.
Fast forward to 2015 and the need for such readily accessible, highly localised and practice-specific information, is even more compelling as health care tends to be delivered by an ever-increasing and ever-changing array of services and teams. In the intervening years technology has transformed how such information may be stored, accessed and updated.
So Spip – a secure online platform inspired by the earlier paper version – has taken over two years for Sara Chambers and Richard Fieldhouse to develop. Both are sessional GPs with over 35 years collective experience of having worked in over 150 different GP surgeries throughout their GP careers.
MPS have supported the development of Spip and CQC have helped with advice.
What is Spip?
Spip is NASGP’s Standardised Practice Induction Portal. It is a secure online platform that enables a practice team to centrally store and safely display essential information to enable any clinician working in any of its premises to manage patients quickly, effectively and efficiently.
It is not linked to your clinical IT system (EMIS, SystmOne etc) and does not contain any patient-identifiable information, so can be shared with any locums visiting your practice and can be accessed from home and on home visits. Within Spip you will find a centrally updatable directory of services – Cudos.
Spip | Who can see the information within Spip and Cudos?
This all depends on what role the Practice has assigned you.
| Role | Spip | Cudos | Group’s Cudos | Explanation |
|---|---|---|---|---|
| Practice | Own & Edit | Own & Edit | View | A single authorised person within the practice who controls and manages Spip and Cudos. Can add and delete contacts in Cudos and content in Spip; can invite anyone to be a Clinician and change the status of Clinician to Editor or Staff. Can also invite and activate Group. |
| Editor | Edit | Edit | View | Same as Clinician; can also add and delete contacts in Cudos as well as in Spip. |
| Staff | View | View | View | Same as Clinician; can also view Cudos. |
| Clinician | View | Hidden | Hidden | Can view all content in Spip that has been authorised for viewing by Practice or Editor. Can not directly view Cudos. |
| network | Dummy | Hidden | Edit | Can only be invited by Practice; can add and delete contacts in a separate Network Cudos. Can not view any contents in Spip. By inviting a Network (e.g. a single contact at a CCG or a GP federation) to add and delete contacts in a separate network Cudos; Practice or Editor can choose to also use contacts that have been added by Network. |
Who owns Spip information?
All information and data added by a practice to a Spip and its corresponding Cudos belongs to that practice. See our Terms and Conditions for more information.
Will any third parties be able to see our Spip data?
Never. The only other people authorised to view your practice’s information are the NASGP’s clinical directors, who will from time-to-time monitor how practices are using their Spips so that NASGP can continually improve Spip.
NASGP is registered with the Data Protection Act.
Is Spip mobile-friendly?
Yes. A Clinician can use Spip from a smartphone using wifi or data (3G or 4G).
What is a Spip ‘Editor’?
The owner of a Spip – ‘Practice’ – can upgrade a Clinician to an Editor.
In addition to everything a Clinician can do, an Editor is also able to populate and edit Spip itself, keeping it up-to-date and relevant.
A Practice can invite as many Clinicians or Staff as it likes to help it ‘crowdsource’ information.
It’s easy to downgrade an Editor back to a Clinician.
How do I use Spip messaging, comments and notes?
Simple, yet powerful
Spip comes with its own messaging, comments and notes system. It’s a great way for all members of a practice – including visiting locum GPs – to share local information about service quality.
If you have any unread messages, we’ll send you an email at 2pm to let you know, allowing you to go straight to your messaging area.
Comment on this page
All users can comment on any page within any Spip they have access too – advice to colleagues, useful tips etc.
That comment will only be visible on that particular practice’s Spip. A copy is sent via the Spip’s messaging system, and the Practice can edit the comment.
Leave a personal note
Useful for Clinicians to leave a personal note about that service for themselves. Only the person who made that note can see it.
Unlike ‘comments’, personal notes will be visible in all other Spips (on that specific page) – but again, visible only to the person who created that note.
Report service issue to Practice
Great for flagging up issues to a Practice about a service, enabling them to collect and escalate these issues further to prevent them happening again.
You must never include any patient-identifiable information in these reports.
Request page update
If you’ve looked something up in Spip but couldn’t find it, or something was out-of-date or wrong, this lets the practice know.
What are the Practice, Staff, Clinician and Editor roles in Spip?
The Practice is the lead role in Spip. This person will have authority from the practice to create a Spip and an NHS email address. They will usually be a practice manager or another senior member of the practice team.
The Practice is able to:
- add and edit items to Spip and Cudos.
- manages other users of Spip and Cudos.
The Practice can invite or deactivate Clinicians:
- The Clinician role can view Spip.
- Clinicians can be any clinician working in your practice who can benefit from access to Spip e.g. practice-based GPs, GP locums and nurses.
The Practice can invite or deactivate Staff:
- Staff can view Spip and Cudos. Cudos may contain items that are just for use by your practice staff e.g. building maintenance, IT system support, health and safety protocols. You would not want to display these in Spip but you can make them accessible to your practice staff by setting them up as Staff roles.
Practice can invite Editors.
- The Editor role can view Spip and Cudos but also add or edit items in Spip or Cudos.
- Editors will usually be established members of your practice team who are entrusted to share their knowledge of practice procedures and services with Clinicians, via Spip, and with Staff via Spip and Cudos e.g. GP partners, medical secretaries and nurse practitioners.
Switching roles
The Practice can switch people between different roles e.g. upgrade a Clinician to an Editor so they can crowdsource their knowledge of services
LocumDeck | Compatibility and security
The entire NASGP website, including Practeus and its associated components LocumDeck, is hosted on a dedicated server, using ISO 27001 and ISO 9001. All data during transmission is encrypted and authenticated using AES 128 GCM and uses ECDHE RSA as the key exchange mechanism.
You do not need to download any software.
If you’re able to, we strongly recommend you upgrade to a modern browser like Google Chrome, Edge, Firefox or Safari to run alongside IE 10 if it’s still needed for NHS legacy websites.
Payment processing
- We do not accept, store, transmit or process cardholder data or any payments. We subcontract all these sensitive payment handling activities to third parties, GoCardless for direct debit payments and Nochex for credit card payments, all of who comply with PCI DSS Standards.
Firewall, security and encryption - Our site uses SHA-256 with RSA Encryption
Cloud server
- LocumDeck is on a dedicated server, which is ISO 27001 security compliant.
Using passwords
The latest advice is to ditch using complex letter/character combinations, and use passphrases instead.
New NIST guidelines recommend using long passphrases instead of seemingly complex passwords. A passphrase is a “memorised secret” consisting of a sequence of words or other text used to authenticate their identity. It’s longer than a password for added security but much easier to learn.
Create unique passphrases you can remember, using whatever characters they want. e.g
- Honeymoon beach flower ketchup
- Correct horse battery staple
How much does Spip cost?
Starting August 2016, Practice Manager membership of the NASGP is now free. Spip comes free with that membership.
Spip has the additional capability to link with any local networks (CCGs, federations, practice hubs etc), for which that network will pay a small monthly charge of no more than £24 for each practice it links to.
It’s also always free to Editors, Clinicians and Staff.
A Practice can:
- Add as many Editors, Clinicians or Staff it needs; although all users have to sign in with an email and a password, they will never have to pay to join the NASGP.
- Cancel their membership at any time.
- Ask us to remove all their data at any time, otherwise we will automatically remove all Spip data after one year. A Practice, and therefore all its Clinicians, Staff etc can re-access its Spip at anytime simply by rejoining.
Can Spip help with CQC compliance?
Yes. Spip is ‘CQC-ready’, with a dedicated section to easily categorise, store and display all your necessary policies.
Spip is a great way to demonstrate to the CQC that the right information is available at the right time to all members of your practice team to allow effective implementation of all your practice procedures. So Spip will not only provide you with a ‘go to’ place for your team to refer to and update information, in creating it, you will also making your CQC compliance less onerous.
See what the CQC has to say about Practice packs.
- Spip allows you to upload, link and add freetext notes for handy summaries and ‘soft intelligence’ about key practice operational procedures. It is a live, interactive, centrally updatable system designed to be easily searched and navigated.
- Once you’re up and running with Spip you will be able to show the CQC that your Staff and Clinicians need never be more than 3 clicks away from information they need.
- GPs can already access key practice policy information that directly affect them as Clinicians e.g. chaperone policy, complaints procedure, clinical handovers, appointment system and access arrangements, practice prescribing procedures, contamination incidents etc.
Managing risk and quality
Monitoring quality of services
- On every Spip page displayed to your team there is a feedback comment system with a prompt to report any problems with a service at the point of use. This intelligence can be collated by the practice for discussion at internal meetings and/or to be raised with the local commissioners and providers.
Patient communication and reducing risk
- Throughout Spip you are prompted to add detailed information about Safety netting, missing results procedures, delayed referrals etc.
- The aim is for everyone in the team to have this information available quickly so that after every patient contact, it is clear to the patient and the practice what is expected next.
Co-operation with other providers of services
Spip is designed to provide up-to-date information which the Clinician can access at the point of need. You have the option of adding enriched information about each service which would equip the Clinician with:
- Awareness of the existence of a service.
- Understanding exactly what the service does; the boundaries of roles and responsibilities between the service and the practice, fostering good team working.
- How to access the service and up-to-date resources to do this e.g. referral forms.
- What to tell the patient about what to expect next.
- Interactive feedback; ability to leave comments or tips for future Clinicians; ability to report a problem with the service; ability to inform you if service details need updating.
How do I create a Spip for a practice?
The person who initially sets up a Spip takes on the lead role, known as ‘Practice’, is responsible for administrative tasks such as managing other Spip users e.g. controlling who can view and edit Spip.
Therefore, usually the practice manager is best placed to initially set up a Spip by registering for Practice Manager membership of the NASGP.
Spip is included free as part of Practice Manager membership.
- You will need an NHS email address ending in
- nhs.net
- nhs.uk
- hscni.net
Once your Spip has been created, you can change your email address to a non-NHS email.
If you are a locum GP who wants to be involved in creating Spips for practices you work in, you can become a ‘Spip Clinician’ by registering with the NASGP as an Associate (free) or Full member. Once signed in, you will be able to ‘Invite new GP practice’ to create a Spip.
If you are a GP wishing to create a Spip for your own practice, unless you want to take on the administrative tasks of managing Spip users, the best route is to ask your practice manager to register for Practice Manager membership and set you up as a ‘Spip Editor’.
Can’t doctors just ask the receptionist?
They – being a GP, nurse, locum or new team member – could just ask the receptionist, but:
- The receptionist may not know the answer. Often this is the case, and a time-consuming game of “pass the parcel” ensues, taking up time of multiple staff. This is no bad reflection on anyone in the practice team; it’s just there’s so much to know and it’s always changing, so it is not reasonable to expect the duty admin team to be ‘know-it-alls’.
- It wastes time – not just the person seeking information (often a GP in the middle of a busy surgery), but the receptionists too.
- It undermines the GP-patient relationship: “If the GP doesn’t even know how to refer me to physiotherapy, how do I know she’s even made the correct diagnosis? I know, I’ll rebook to see another GP.”.
If we’ve already got DXS/Map of Medicine, why do we need Spip?
Think of Spip as the information air traffic control of your GP practice, while services like DXS and Map of Medicine are the different airlines. Information used in GP practices comes from many different internal and external sources, and DXS/Map of Medicine are only one of these, and are generally outside the control of the practice.
Spip is practice-specific, focused on enabling a Clinician at the point of use to run a safe, effective and efficient consultation, or a Staff member referring to up-to-date information about practice processes. This encompasses far more than is contained in a local guideline.
For example, a local guideline may simply state “Arrange urgent ultrasound scan”. Enacting this seemingly simple instruction will actually involve the Clinician having access to lots of bits of information about how your practice works:
- How do I organise an urgent ultrasound in this practice?
- Do I just send a form or do I also have to phone radiology?
- Where are the referral forms?
- How does this practice handle urgent referrals?
- What’s this practice’s policy on informing the patient of the results?
Spip:
- Is completely controlled by you and is centred around your practice rather than the CCG.
- Does not require an NHS smartcard, and is not integrated into the clinical system. So it can be accessed by any clinician from a smartphone or from home, during visits, and before visiting a practice for locum work for the first time – or any time!
- Uses a standardised format – all practice Spips have exactly the same structure – which is quick and easy to navigate, so you can direct Clinicians to key information about how your practice works and how you link up to local guidelines.
How does a GP invite a practice to set up a Spip?
Click on the Choose Practice Pack logo (you’ll need to sign in if you’ve not already done so) and select Invite new GP practice.
You can invite as many practices to set up a Spip as you like.
How does Spip help clinicians work better?
When it comes to managing a patient in a GP surgery, we need access to one of atleast 200 items of information that are specific to that practice. If we can’t recall this from memory, or it’s not immediately accessible, retrieving this information can waste precious minutes or even hours of our time, a colleagues time and , most importantly, our patients time and even put a patient’s health at risk.
It’s those 200 bits of local, practice-based, non-clinical information that Spip enables practices to provide for all clinicians caring for their patients:
- How do I organise an urgent ECG in the middle of a busy surgery?
- What do I tell a patient about how they will be informed of abnormal blood tests?
- Which helicobacter pylori test is used at this practice?
- I’ve seen a nine year old boy with suspected testicular torsion who needs emergency referral. Which team do I refer him to?
- The local DVT pathway says ‘Do a D-dimer test’. How is this done at this practice?
- Where are echocardiograms carried out? How do I request one? What do I tell the patient about the appointment-making process?
- I’ve requested a chest x-ray on a 68 year old man with a cough. How do I alert his usual GP that he may have a significant diagnosis?
- What’s the extension number for main reception?
- Who’s the practice’s child safeguarding lead?
- I need a foreign language interpreter.
- How do I organise an urgent coil fitting as emergency contraception?
- What’s the door access code to the toilet?
Spip contains over 200 similar, simple-yet-essential everyday scenarios.
Toolkit | Checklist for home visits
Home visits are some of the most complicated activities that GPs do. Away from electronic records, usually after a busy surgery, through traffic, to sick or frail patients, often with multiple problems and anxious carers.
Our template helps you make the whole process go much more smoothly.
Checklist for home visits
Download – Word Save as – Google Doc
See also
Toolkit | Restock consulting room equipment
The best person to let you know when a room needs reequipping is the last person that used it. Print some of these out and pin to each room’s notice board.
Restock consulting room equipment
Toolkit | Locum pre-arrival checklist
To get the most out of your freelance GPs and minimise stress to your practice staff and disruption for patients, it is helpful to have the following in place in time for your GPs to smoothly start their session.
Locum pre-arrival checklist
Download – Word Save as – Google Doc
See also – More tools for practices to support locums
Toolkit | Dictate referral template
These allow clinicians to make a physical record of every consultation that needs referral, reducing the likelihood of a referral going missing.